191x Filetype PDF File size 2.23 MB Source: www.sahta.com
January 2015 Volume 38, Supplement 1
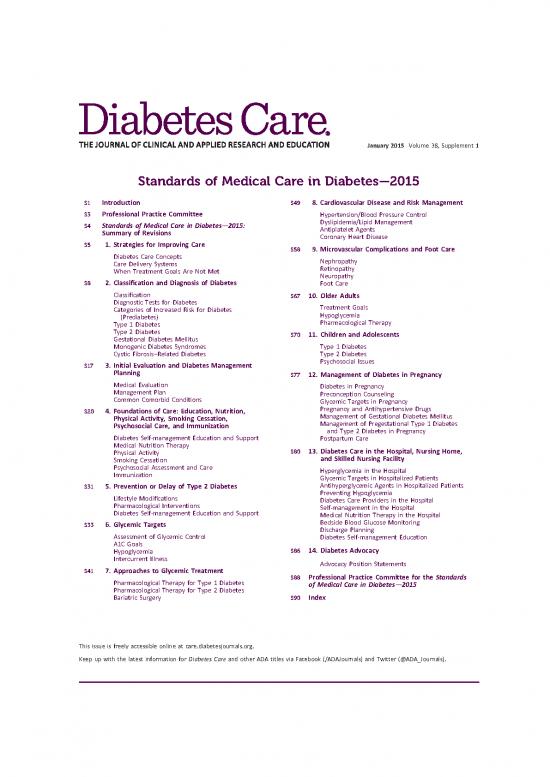
Standards of Medical Care in Diabetes—2015
S1 Introduction S49 8. Cardiovascular Disease and Risk Management
S3 Professional Practice Committee Hypertension/Blood Pressure Control
S4 Standards of Medical Care in Diabetes—2015: Dyslipidemia/Lipid Management
Summary of Revisions Antiplatelet Agents
Coronary Heart Disease
S5 1. Strategies for Improving Care S58 9. Microvascular Complications and Foot Care
Diabetes Care Concepts Nephropathy
Care Delivery Systems Retinopathy
When Treatment Goals Are Not Met Neuropathy
S8 2. Classification and Diagnosis of Diabetes Foot Care
Classification S67 10. Older Adults
Diagnostic Tests for Diabetes Treatment Goals
Categories of Increased Risk for Diabetes Hypoglycemia
(Prediabetes) Pharmacological Therapy
Type 1 Diabetes
Type 2 Diabetes S70 11. Children and Adolescents
Gestational Diabetes Mellitus
Monogenic Diabetes Syndromes Type 1 Diabetes
Cystic Fibrosis–Related Diabetes Type 2 Diabetes
S17 3. Initial Evaluation and Diabetes Management Psychosocial Issues
Planning S77 12. Management of Diabetes in Pregnancy
Medical Evaluation Diabetes in Pregnancy
Management Plan Preconception Counseling
Common Comorbid Conditions Glycemic Targets in Pregnancy
S20 4. Foundations of Care: Education, Nutrition, Pregnancy and Antihypertensive Drugs
Physical Activity, Smoking Cessation, Management of Gestational Diabetes Mellitus
Psychosocial Care, and Immunization Management of Pregestational Type 1 Diabetes
and Type 2 Diabetes in Pregnancy
Diabetes Self-management Education and Support Postpartum Care
Medical Nutrition Therapy
Physical Activity S80 13. Diabetes Care in the Hospital, Nursing Home,
Smoking Cessation and Skilled Nursing Facility
Psychosocial Assessment and Care Hyperglycemia in the Hospital
Immunization Glycemic Targets in Hospitalized Patients
S31 5. Prevention or Delay of Type 2 Diabetes Antihyperglycemic Agents in Hospitalized Patients
Lifestyle Modifications Preventing Hypoglycemia
Pharmacological Interventions Diabetes Care Providers in the Hospital
Diabetes Self-management Education and Support Self-management in the Hospital
Medical Nutrition Therapy in the Hospital
S33 6. Glycemic Targets Bedside Blood Glucose Monitoring
Discharge Planning
Assessment of Glycemic Control Diabetes Self-management Education
A1C Goals
Hypoglycemia S86 14. Diabetes Advocacy
Intercurrent Illness Advocacy Position Statements
S41 7. Approaches to Glycemic Treatment
S88 Professional Practice Committee for the Standards
Pharmacological Therapy for Type 1 Diabetes of Medical Care in Diabetes—2015
Pharmacological Therapy for Type 2 Diabetes
Bariatric Surgery S90 Index
This issue is freely accessible online at care.diabetesjournals.org.
Keep up with the latest information for Diabetes Care and other ADA titles via Facebook (/ADAJournals) and Twitter (@ADA_Journals).
Diabetes Care Volume 38, Supplement 1, January 2015 S1
I
NTR
OD
UCT
I
ON
Introduction
Diabetes Care 2015;38(Suppl. 1):S1–S2 | DOI: 10.2337/dc15-S001
Diabetesisacomplex,chronicillnessre- ADASTANDARDS, STATEMENTS, ADAScientific Statement
quiring continuous medical care with ANDREPORTS A scientific statement is an official
multifactorial risk-reduction strategies The ADA has been actively involved in ADApoint of view or belief that may or
beyond glycemic control. Ongoing pa- the development and dissemination of maynotcontainclinical or research rec-
tient self-management education and diabetescarestandards,guidelines, and ommendations. Scientificstatements
support are critical to preventing acute related documents for over 20 years. contain scholarly synopsis of a topic re-
complications and reducing the risk of ADA’s clinical practice recommenda- lated to diabetes. Workgroup reports
long-term complications. Significant tions are viewed as important resources fall into this category. Scientific state-
evidence exists that supports a range for health care professionals who care ments are published in the ADA journals
of interventions to improve diabetes for people with diabetes. ADA’s “Stan- andother scientific/medical publications,
outcomes. dards of Medical Care in Diabetes,” as appropriate. Scientific statements also
The American Diabetes Association’s position statements, and scientific undergo a formal review process.
(ADA’s) “Standards of Medical Care in statements undergo a formal review
Diabetes” is intended to provide cli- process by ADA’s Professional Practice Consensus Report
nicians, patients, researchers, payers, Committee (PPC) and the Executive A consensus report contains a compre-
and other interested individuals with Committee of the Board of Directors. hensive examination by an expert panel
the components of diabetes care, gen- The Standards and all ADA position state- (i.e., consensus panel) of a scientificor
eral treatment goals, and tools to eval- ments,scientificstatements,andconsensus medicalissuerelatedtodiabetes.Acon-
uate the quality of care. The Standards reports are available on the Association’s sensusreportisnotanADApositionand
of Care recommendations are not in- Website at http://professional.diabetes.org/ represents expert opinion only. The cat-
tended to preclude clinical judgment adastatements. egory may also include task force and
and must be applied in the context of expert committee reports. The need
excellent clinical care, with adjustments “Standards of Medical Care in Diabetes” for a consensusreportariseswhenclini-
for individual preferences, comorbid- Standards of Care: ADA position state- cians or scientists desire guidance on
ities, and other patient factors. For ment that provides key clinical practice a subject for which the evidence is con-
more detailed information about man- recommendations.ThePPCperformsan tradictory or incomplete. A consensus
agement of diabetes, please refer to extensive literature search and updates report is typically developed immedi-
Medical ManagementofType1Diabetes the Standards annually based on the ately following a consensus conference
(1) and Medical Management of Type 2 quality of new evidence. where the controversial issue is exten-
Diabetes (2). sively discussed. The report represents
The recommendations include screen- ADAPosition Statement the panel’s collective analysis, evalua-
ing, diagnostic, and therapeutic actions A position statement is an official ADA tion, and opinion at that point in time
that are known or believed to favor- pointofvieworbeliefthatcontainsclinical based in part on the conference pro-
ablyaffecthealthoutcomesofpatients or research recommendations. Position ceedings. A consensus report does not
with diabetes. Many of these interven- statementsareissuedonscientificormed- undergo a formal ADA review process.
tionshavealsobeenshowntobecost- ical issues related to diabetes. They are
effective (3). publishedinADAjournalsandotherscien- GRADINGOFSCIENTIFICEVIDENCE
TheADAstrivestoimproveandupdate tific/medical publications. ADA position Since the ADA first began publishing
theStandardsofCaretoensurethatclini- statements are typically based on a sys- practice guidelines, there has been con-
cians, health plans, and policy makers can tematic review or other review of pub- siderable evolution in the evaluation of
continue to rely on them as the most au- lished literature. Position statements scientific evidence and in the develop-
thoritative and current guidelines for di- undergo a formal review process. They ment of evidence-based guidelines.
abetes care. are updated annually or as needed. In 2002, we developed a classification
“Standards of Medical Care in Diabetes” was originally approved in 1988. Most recent review/revision: October 2014.
©2015bytheAmericanDiabetesAssociation.Readersmayusethisarticleaslongastheworkisproperlycited,theuseiseducationalandnotforprofit,
and the work is not altered.
S2 Introduction Diabetes Care Volume 38, Supplement 1, January 2015
Table1—ADAevidence-gradingsystemfor“StandardsofMedicalCareinDiabetes” recommendationshavethebestchance
Level of of improving outcomeswhenappliedto
evidence Description thepopulationtowhichtheyareappro-
A Clear evidence from well-conducted, generalizable randomized controlled priate. Recommendations with lower
trials that are adequately powered, including levelsofevidencemaybeequallyimpor-
c Evidence from a well-conducted multicenter trial tant but are not as well supported.
c Evidence from a meta-analysis that incorporated quality ratings in the Of course, evidence is only one com-
analysis ponentofclinicaldecisionmaking.Clini-
Compelling nonexperimental evidence; i.e., “all or none” rule developed by cians care for patients, not populations;
the Centre for Evidence-Based Medicine at the University of Oxford guidelines must always be interpreted
Supportive evidence from well-conducted randomized controlled trials that with the individual patient in mind.
are adequately powered, including Individual circumstances, such as co-
c Evidence from a well-conducted trial at one or more institutions
c Evidence from a meta-analysis that incorporated quality ratings in the morbidandcoexistingdiseases,age,ed-
analysis ucation, disability, and, above all,
B Supportive evidence from well-conducted cohort studies patients’ values and preferences, must
c Evidence from a well-conducted prospective cohort study or registry beconsideredandmayleadtodifferent
c Evidence from a well-conducted meta-analysis of cohort studies treatment targets and strategies. Also,
Supportive evidence from a well-conducted case-control study conventional evidence hierarchies, such
C Supportive evidence from poorly controlled or uncontrolled studies as the one adapted by the ADA, may
c Evidence from randomized clinical trials with one or more major or three miss nuances important in diabetes
or more minor methodological flaws that could invalidate the results care. For example, although there is ex-
c Evidence from observational studies with high potential for bias (such as
case series with comparison with historical controls) cellent evidence from clinical trials sup-
c Evidence from case series or case reports porting the importance of achieving
Conflicting evidence with the weight of evidence supporting the multiple risk factor control, the optimal
recommendation waytoachieve this result is less clear. It
E Expert consensus or clinical experience is difficult to assess each component of
such a complex intervention.
system to grade the quality of scienti- and codify the evidence that forms the References
ficevidencesupportingADArecommen- basis for the recommendations. 1. Kaufman FR (Ed.). Medical Management of
dations for all new and revised ADA ADA recommendations are assigned Type 1 Diabetes, 6th ed. Alexandria, VA, Amer-
position statements. A recent analysis ratings of A, B,orC, depending on the ican Diabetes Association, 2012
of the evidence cited in the Standards qualityofevidence.ExpertopinionEisa 2. Burant CF (Ed.). Medical Management of
of Care found steady improvement in separatecategoryforrecommendations Type 2 Diabetes, 7th ed. Alexandria, VA, Amer-
quality over the past 10 years, with last in which there is no evidence from clin- ican Diabetes Association, 2012
3. Li R, Zhang P, Barker LE, Chowdhury FM,
year’sStandardsforthefirsttimehaving ical trials, in which clinical trials may Zhang X. Cost-effectiveness of interventions to
the majority of bulleted recommenda- beimpractical, or in which there is con- preventandcontroldiabetesmellitus:asystem-
tions supported by A-orB-level evi- flicting evidence. Recommendations atic review. Diabetes Care 2010;33:1872–1894
dence (4). A grading system (Table 1) with an A rating are based on large 4. Grant RW, Kirkman MS. Trends in the evi-
dence level for the American Diabetes Associa-
developed by ADA and modeled after well-designed clinical trials or well- tion’s “Standards of Medical Care in Diabetes”
existing methods was used to clarify done meta-analyses. Generally, these from 2005 to 2014. Diabetes Care 2015;38:6–8
P
Diabetes Care Volume 38, Supplement 1, January 2015 S3 RO
FE
SS
IO
NAL
PR
A
CTI
CE
CO
Professional Practice Committee MMI
Diabetes Care 2015;38(Suppl. 1):S3 | DOI: 10.2337/dc15-S002 TT
EE
The Professional Practice Committee for human studies related to each sec- EdwardW.Gregg,PhD;SilvioE.Inzucchi,
(PPC) of the American Diabetes Associa- tionandpublishedsince1January2014. MD; Mark E. Molitch, MD; John M.
tion (ADA) is responsible for the “Stan- Recommendations were revised based Morton, MD; Robert E. Ratner, MD;
dards of Medical Care in Diabetes” on new evidence or, in some cases, to Linda M. Siminerio, RN, PhD, CDE; and
position statement, referred to as the clarify the prior recommendation or Katherine R. Tuttle, MD.
“StandardsofCare.”ThePPCisamultidis- match the strength of the wording to
ciplinary expert committee comprised of thestrengthoftheevidence.Atablelink- MembersofthePPC
physicians, diabetes educators, registered ing the changes in recommendations to
dietitians, and others who have expertise newevidencecanbereviewedathttp:// Richard W. Grant, MD, MPH (Chair)*
in a range of areas, including adult and professional.diabetes.org/SOC. As for ThomasW.Donner,MD
pediatric endocrinology, epidemiology, all position statements, the Standards Judith E. Fradkin, MD
publichealth,lipidresearch,hypertension, of Care position statement was reviewed
and preconception and pregnancy care. andapprovedbytheExecutiveCommittee Charlotte Hayes, MMSc, MS, RD, CDE,
AppointmenttothePPCisbasedonexcel- of ADA’s Board of Directors, which in- ACSMCES
lence in clinical practice and/or research. cludeshealthcareprofessionals,scientists, William H. Herman, MD, MPH
While the primary role of the PPC is to and lay people. William C. Hsu, MD
review and update the Standards of Feedback from the larger clinical Eileen Kim, MD
Care, it is also responsible for overseeing community was valuable for the 2015
the review and revisions of ADA’sposition revision of the Standards of Care. Read- Lori Laffel, MD, MPH
statements and scientificstatements. ers who wish to comment on the Stan- Rodica Pop-Busui, MD, PhD
All members of the PPC are required dards of Medical Care in Diabetesd2015 Neda Rasouli, MD*
to disclose potential conflicts of interest are invited to do so at http://professional
with industry and/or other relevant or- .diabetes.org/SOC. DesmondSchatz, MD
ganizations. These disclosures are dis- The ADA funds development of the Joseph A. Stankaitis, MD, MPH*
cussed at the onset of each Standards Standards of Care and all ADA position Tracey H. Taveira, PharmD, CDOE,
of Care revision meeting. Members of statements out of its general revenues CVDOE
the committee, their employer, and and does not use industry support for
their disclosed conflicts of interest are these purposes. Deborah J. Wexler, MD*
listed in the “Professional Practice Com- The PPC would like to thank the fol- *Subgroup leaders
mittee for the Standards of Medical lowing individuals who provided their ex-
Care in Diabetesd2015” table (see pertise in reviewing and/or consulting with ADAStaff
p. S88). the committee: Donald R. Coustan, MD;
For the current revision, PPC mem- Stephanie Dunbar, MPH, RD; Robert H. Jane L. Chiang, MD
bers systematically searched MEDLINE Eckel, MD; Henry N. Ginsberg, MD; Erika Gebel Berg, PhD
©2015bytheAmericanDiabetesAssociation.Readersmayusethisarticleaslongastheworkisproperlycited,theuseiseducationalandnotforprofit,
and the work is not altered.
no reviews yet
Please Login to review.