126x Filetype PDF File size 0.63 MB Source: www.hrpub.org
Cancer and Oncology Research 6(1): 11-25, 2020 http://www.hrpub.org
DOI: 10.13189/cor.2020.060102
Nutritional Considerations in Childhood Acute
Lymphoblastic Leukemia
1,2,* 2
Sami El Khatib , Mona Omar
1Department of Biomedical Sciences, School of Arts & Sciences, Lebanese International University, Lebanon
2Department of Biological Sciences, School of Arts & Sciences, Lebanese International University, Lebanon
Received December 8, 2019; Revised January 19, 2020; Accepted February 7, 2020
Copyright©2020 by authors, all rights reserved. Authors agree that this article remains permanently open access under the
terms of the Creative Commons Attribution License 4.0 International License
Abstract The high prevalence of malnutrition in adult cells. There are more than 100 type of cancer including breast
and pediatric cancer patients has been appreciated for cancer, skin cancer, lung cancer, colon cancer, prostate
decades and continues to be documented. Although the cancer, and lymphoma. Symptoms vary on the type. The
prognostic significance of nutritional status among patients treatment may include chemotherapy, radiation, and surgery.
with cancer remains controversial, it is generally accepted Many search articles and clinical trials were conducted under
that the nutritional support is an important aspect of medical the title of oncology aiming at exploring cancer cell behavior
therapy. Children with cancer are particularly vulnerable to and discovering the most optimal cure. It’s every researcher’s
malnutrition, because they exhibit elevated substrate needs dream. This research investigates the nutritional role or in
due to the disease and its treatment. At the same time, other words its impact on cancer growth and prognosis aside
children have increased requirements of nutrients to attain by the conventional treatment. The current review shed the
appropriate growth and neurodevelopment. Malnutrition in light over the nutritional management effect on patients with
children with cancer should not be accepted at any stage of cancer during therapy and afterward. The manuscript
the disease or tolerated as an inevitable process. The includes firstly an overview about the most relevant type of
undernourished patients of ALL are more prone to infections, childhood cancer which is leukemia and indicating the
requiring longer duration of hospital stay. Therefore, optional treatments. We thereafter incorporate few nutrition
optimum nutritional support to such patients can help to considerations as malnutrition effect on treatment results,
decrease the chances of infections and ultimately improve the serum zinc and copper role in malignancy, supplement of
outcome based on a systematic assessment. Nutritional folate and B in deficient patients, mucositis and sinusoidal
12
assessment is the first step of nutritional support which will obstructive syndrome, drug and nutrient interaction, and
not improve the child's sense of well-being but also maintain oxidative stress. Glutamine, antioxidant, and other dietary
normal growth, promote wound healing, improve tumor supplements that might lift up the treatment overall outcome
response to therapy and enable the child to better withstand with less side effects are then highlighted. Nutrition
the effects of therapy. Assessment will also help prevent over ingredients are becoming the new breakthrough in medical
nutrition which may in some instances be detrimental to the remedies as sulforaphane and garlic compounds among the
treatment of cancer. Therefore, nutritional adequate adopted nutritional recommendations pinpointed hereby.
strategies should be considered and integrated as a
fundamental feature of pediatric oncology with the same
diligence as one does for other supportive care measures to 2. Acute Lymphoblastic Leukemia and
prevent chronic illness and adverse late effects caused by Treatment Options
malnutrition in children with ALL.
Keywords Pediatric Nutrition, Acute Lymphoblastic 2.1. Overview of Leukemia
Leukemia, Malnutrition, Oncology, Childhood ALL
Cancer is a disorder in cells regulatory system and
development leading to the formation of abnormal cell
division and production. Cancer can almost start anywhere in
1. Introduction the human body. These unregulated cells may spread to other
organs and tissues, thus turning into cancer or become
Cancer also termed malignancy is an abnormal growth of situational tumor (Owens, 2013).
12 Nutritional Considerations in Childhood Acute Lymphoblastic Leukemia
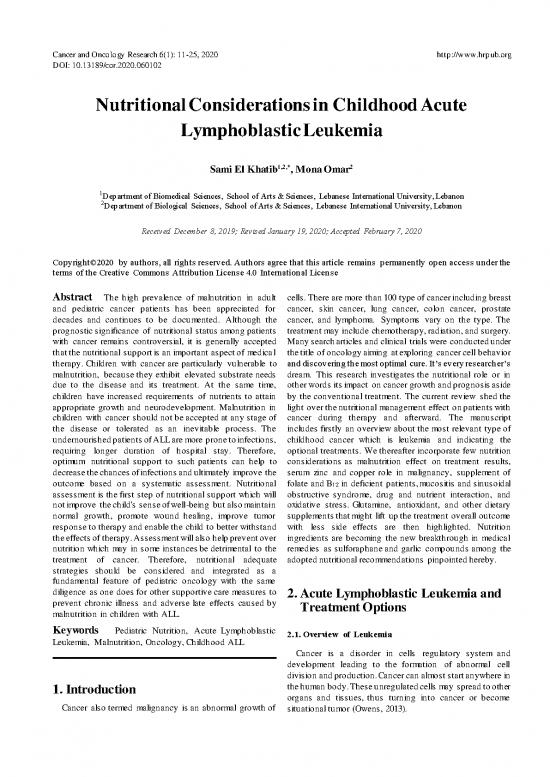
Figure 1. Blood cell development. A blood stem cell goes through several steps to become a red blood cell, platelet, or white blood cell (PDQ, 2016)
Leukemia is one of the many forms that cancer might take. leukemia, chronic myeloid leukemia, acute lymphocytic
It originates in the bone marrow and liberates to the blood leukemia (ALL), acute myeloid leukemia are common types
steam. In a healthy child, the bone marrow produces blood of leukemia of which ALL is the most common type of
stem cell (immature cells) that becomes mature over time. cancer in children (Owens, 2013).
These stem cells may assume a form of myeloid stem cell or 2.1.1. Incidence of ALL
a lymphoid stem cell. Myeloid stem cells are transformed to
either one of the three types of mature blood cells: White children ALL incidences are approximately three
Red blood cells (RBC) that is responsible of times higher than in Black children from ages 2 to 3 years
transporting oxygen to other substances to all body old. Meanwhile the overall incidence of ALL has been
tissues and organs. increasing slowly in the past decades. For instance, it is
Platelets, which forms blood clots in order to cause nearly about 30 to 40 case in every 1 million in pediatrics
bleeding. under the age of 20 years old in the United States (Owens,
White blood cells (WBC), which partition in bodies 2013). Each year relatively 3100 US people who are under
defense against infections and diseases. They are the age of 20 are diagnosed with ALL. It is greater seen in
monocytes and granulocytes (eosinophils, basophils, who are 10 years old and above than in infants and 8 years
and neutrophils), as demonstrated in figure 1. old (PDQ, 2016). A 34 incident in every 1 million shows to
A lymphoid stem cells turns into a lymphoblast cell, then have ALL in Hispanic children as it appears to be the greatest
into lymphocyte (WBC): incidence (PDQ, 2016).
B lymphocytes, that produces antibodies 2.1.2. Causes and Risk Factors
T lymphocytes, that acids B lymphocytes to make There is no one causative factor has been associated or link
antibodies for fighting infections to cancer development; meanwhile some risk factors are
Natural killer cells (NK cells), that attack tumor cells identified to increase of ALL risk. Some of them include the
and virus-infected cells (PDQ, 2016) following:
Leukemia cells are a term given to cancerous cells Prenatal exposure to X-rays.
produced from either myeloid or lymphoid cell lines. This Exposure to radiation, such as therapeutic radiation
term is later divided into acute (rapid onset and progression) used for thymus enlargement for example.
or chronic (slow onset and progression) malignant cells. It is Past chemotherapy treatment.
further sub-divided to lymphoid (lymphocytic or Genetic conditions, that can be detected in 75% to 80%
lymphoblastic) or myeloid cells. Chronic lymphocytic of all childhood ALL (Owens, 2013), as:
Cancer and Oncology Research 6(1): 11-25, 2020 13
Down syndrome, also known as trisomy 21, a WBC count <50000/µl at diagnosis) or a high-risk (WBC
condition in which extra genetic material cause count ≥50000/µl at diagnosis). In addition of assuming of
delays in child’s development mentally and what is prognosis might be like. With that being said the team;
physically. entrusted group to treat and follow-up disease progression
Neurofibromatosis (NFI mutation) a genetic and outcome; incorporates all the necessary skills and
disorder in which neurofibromas from throughout assistance from the health care professionals to ensure that
nervous system. patients are receiving the right treatment, care and
Blood syndrome (BLM gene mutation), an rehabilitation to achieve optimal survival and quality of life
inherited disorder characterized by short stature a (PDQ, 2016; PDQ patient’s overview, 2016).
skin rash that develops after exposure to the sun Phases of therapy are divided into:
and greatly increased risk of cancer. 1. Remission induction phase.
Ataxia-telangiectasia (ATM gene mutation), refers 2. Consolidation/ intensification phase.
to as Louis-bar syndrome, a rare 3. Maintenance or continuation phase (PDQ, 2016; PDQ
neurodegenerative autosomal recessive disease patient’s overview, 2016).
causing severs disability. Ataxia refers to poor 2.2.1. Induction Phases
coordination and telangiectasia is a small dilated
In remission induction chemotherapy, the first phase of
blood vessel (hall marks of disease). Li-Frawmeni
treatment of a 4-week duration. Its main goal is to abet a full
syndrome, constitutional mismatch repair
remission. This is accomplished by using drugs to kill
deficiency, low-and-high-penetrance inherited
leukemia cells wherever they exist in the body. This phase
genetic variants, and Fanconi anemia are other typically consists of the following drugs with or without
genetic disorders (PDQ, 2016).
2.1.3. Signs and Symptoms anthracycline (daunorubian or doxorubicin):
Vincristine, a plant alkaloid used in the management of
The increasing number of leukemia cells in blood and bone leukemia and lymphomas. It is an anti-cancer
marrow leads to a narrower spaces left for WBC, RBC, and (antineoplastic or cytotoxic).
platelets causing infections, anemia, and bleeding. Other Corticosteroid, either prednisone or dexamethasone,
signs and symptoms include malaise, lymph node were dexamethasone has more favorable outcomes.
enlargement, bone or joint pain, fever, pallor, loss of appetite, Acting as anti-inflammatory, anti-neoplastic and
petechial, abdominal discomfort (pain, feeling of fullness immunosuppressive.
below ribs), and swelling (Owens, 2013). L-asparaginase, which is classified as an enzyme and
several forms like pegaspargase (PEG-asparaginase),
2.1.4. Diagnosis
Erwiana L-asparaginase, and native Escherichia coli L-
Tests and procedures are used to distinguish childhood asparaginase are used in the treatment. Putting into
ALL, and to check if cancer cells have spread to other body consideration those patients who are allergic to
organs or tissues. The diagnosis includes a physical pegaspargase be compelled to use Erwiana L-
examination to assess lumps existence or anything else that asparaginase (PDQ, 2016).
seems unusual. Checking the medical history of the patient 2.2.2. Consolidation & Intensification Phase (Therapy)
also comes in favor. A complete blood count (CBC) where a This second phase of treatment aims at eliminating any
blood sample is drawn and examined for any abnormality in remaining leukemia cells in the body to avoid relapse. It
number of RBC, platelets, and WBC with these types, as well begins once the leukemia is in remission and in conjunction
for anemia checking. Measuring blood chemistry for specific with central nervous system-directed therapy. The risk group
substances released by some organs into the blood and implies the intensity of post induction therapy (PDQ, 2016).
comparing them to usual concentrations for detection of BFM (Berlin Frankfurt Munster) backbone is the most
certain diseases. Even with the enhanced production of adopted intensification schema, and it includes the following:
undifferentiated blast cells, the main confirmation for the 1. Initial consolidation, immediately following the
occupation of leukemia cells in the bone marrow is through
completion of a bone marrow aspiration or biopsy. Lumbar complete remission phases. Where cyclophosphamide,
puncture and chromosomal analysis are used to specify the low-dose without leucovorin rescue are being used and
type of leukemia (Owens, 2013). mercaptopurine are used.
2. Interim maintenance phases, where multiple doses of
2
2.2. Chemotherapy high-doses methotrexate (5g/m ) with leucovorin
rescue or escalating doses of methotrexate (starting
2
Before tackling the treatment options of children with dose 100 mg/m ) without leucovorin rescue are being
ALL, the treating group of experts must put into used.
consideration the child age, gender, race which WBC 3. Reduction, which follows a similar order of drugs and
leukemia has originated from as well any genetic changes in timing that is used during induction and initial
lymphocytes whether the child has a standard-risk (with consolidation rounds.
14 Nutritional Considerations in Childhood Acute Lymphoblastic Leukemia
4. Maintenance, of daily mercaptopurine a weekly low- cranial nerve palsies. An overt-CNS leukemia will flourish in
dose methotrexate and sometimes administration of most children where or not lymphoblast was detected in the
vincristine and a corticosteroid, as well as continued spinal fluid at primary diagnosis, except a specific therapy is
intrathecal therapy (PDQ, 2016). conducted towards the CNS. Consequently, ALL are to
2.2.3. Maintenance Phase receive a combination therapy with CNS prophylaxis. Due to
the fact that CNS is sanctuary early directed treatment are
The third phase shoots at extermination of leukemia cells launched early to eliminate clinically evident CNS diseases
that may have survived the previous phases of treatments to upon diagnosis and to baffle CNS relapse in all patients (PDQ,
avoid risk of relapse. Generally, maintenance chemotherapy 2016).
continues 2 to 3 years along with cranial radiation (CR) Standard treatment options include:
continuation. Extending it beyond 3 years has no favorable 1. Intrathecal chemotherapy: usually starts at the
outcomes. A standard protocol accommodates daily oral beginning of induction phases, and continuous
mercaptopurine and weekly oral or parenteral methotrexate, throughout maintenance phases but with variable
nevertheless non-compliance of adherence to these lessened intensities. It may use methotrexate alone or in addition
drug dosages are associated with significant risk of relapse. with cytarabine and hydrocortisone forming triple
Therefore, a careful monitoring of children by the medical intrathecal chemotherapy. Intrathecal methotrexate has
team is critical at all times (PDQ, 2016). significant systemic effect that contributes to marrow
The administration of drugs can be done by two means, a relapse prevention may have been noticed.
mouth or vein. If the chemotherapeutic drug or drugs are 2. CNS-directed systemic chemotherapy: it
directly administered into the target area where leukemia systemically delivers agents that own some properties.
cells are located it’s then called regional chemotherapy, such The following drugs include dexamethasone, L-
as intrathecal chemotherapy. Meanwhile allocating drugs asparaginase, high dose methotrexate with leucovirin
into the blood stream spreading throughout the body to reach rescue, escalating IV methotrexate dose without
its target cells is systemic chemotherapy. Putting into leucovirin rescue.
consideration that high-risk ALL children acquire more 3. Cranial improvement: a high energy x-rays or gamma
intensified therapy where they include more anti-cancer rays are used to destroy leukemia cells. It’s used for
drugs with high doses than low-risk ALL patients (PDQ special cases and high risk CNS leukemia.
patient’s overview, 2016). A dramatic improvement was shown as CNS-directed
2.3. CNS-Directed Therapy for Childhood ALL therapies were combined with treatment regimens. Usually
intrathecal chemotherapy combined with CNS-directed
Almost 3% of children appear to have central nervous systemic chemotherapy is standard and commonly used for
system 3 (CNS3) diseases upon diagnosis. CNS3 is noted by newly diagnosed ALL children as presented in table 1. As for
the detection of 5 or more WBC found in the cerebrospinal cranial radiation it is selective (PDQ, 2016).
fluid (CNF) specimen in addition to presence or absence of
Table 1. CNS-Directed Treatment Regimens for Newly Diagnosed Childhood ALL (PDQ, 2016)
Standard Treatment Options Standard-risk ALL Patient High-risk ALL Patient
Methotrexate alone. Methotrexate alone.
Intrathecal chemotherapy Methotrexate with Cytarabine and Methotrexate with Cytarabine and
Hydrocortisone. Hydrocortisone.
Dexamethanose.
L-asparaginase. Dexamethanose.
CNS-directed systemic High-dose methotrexate with Leucovorine L-asparaginase.
chemotherapy rescue. High-dose methotrexate with
Escalating-dose intravenous methotrexate (no Leucovorine rescue.
leucovorine rescue).
Cranial radiation No Yes
no reviews yet
Please Login to review.