216x Filetype PDF File size 0.16 MB Source: brieflands.com
IranJPsychiatryBehavSci.2020September;14(3):e101535. doi: 10.5812/ijpbs.101535.
Publishedonline2020August4. ResearchArticle
Effectivenessof Exposure/ResponsePreventionplusEyeMovement
DesensitizationandReprocessinginReducingAnxietyand
Obsessive-CompulsiveSymptomsAssociatedwithStressfulLife
Experiences: ARandomizedControlledTrial
MohammadEbrahimSarichloo 1,FarhadTaremian 1, 2, *, Behrouz Dolatshahee 1, 2 and Seyed
AlirezaHajiSeyedJavadi 3
1DepartmentofClinicalPsychology,Universityof SocialWelfareandRehabilitationSciences,Tehran,Iran
2SubstanceAbuseandDependenceResearchCenter,UniversityofSocialWelfareandRehabilitationSciences,Tehran,Iran
3DepartmentofPsychiatry,QazvinUniversityofMedicalSciences,Qazvin,Iran
*Correspondingauthor:SubstanceAbuseandDependenceResearchCenter,UniversityofSocialWelfareandRehabilitationSciences,Tehran,Iran.Tel:+98-2171732841,
+98-2171732845,Email: fa.taremian@uswr.ac.ir
Received2020March28;Revised2020May02;Accepted2020June19.
Abstract
Background:Obsessive-compulsivedisorder(OCD)isknownasanon-psychoticmentaldisorderresistanttotreatment.Ithasbeen
foundthateyemovementdesensitizationandreprocessing(EMDR)canincreasetheeffectivenessofitsstandardtreatments.
Objectives: The current study aimed at evaluating the impact of exposure/response prevention (ERP) combined with EMDR as a
treatmentmethodonpatientswithOCDwhohadexperiencedstressfullifeeventsbycomparisontoERPalone.
Methods: Thepresentrandomizedcontrolledtrial was conducted among 60 OCD patients who experienced stressful life events
andwereresistanttomedicationtreatment. TheparticipantswererandomlyassignedtotheERPplusEMDR(n=30)andERP(n=
30)groups.TheYale-BrownObsessive-Compulsivescale(Y-BOCS)andBeckAnxietyInventory(BAI)werecompletedbeforeandafter
theintervention,aswellas,afterafollow-upperiodofthreemonths.Thescoreswerecomparedusingthechi-squaredtest,analysis
of covariance(ANCOVA),andrepeatedmeasuresanalysisofvariance(ANOVA).
Results:ANOVAresultsdemonstratedthatbothtreatmentprotocolshadasignificanteffectonthereductionofanxietyandseverity
of OCDsymptoms,whiletheresultsofANCOVAshowedasignificantlyhighereffectofERPplusEMDRcomparedtotheERPprotocol
(P=0.001),andsampleattritionwassignificantlyhigherintheERPgroup(P< 0.05).
Conclusions: TheERPplusEMDRprotocolcomparedtotheERPprotocolshowedahigherrateof completionandefficacyinOCD
treatment.
Keywords:Anxiety,Exposure/ResponsePrevention,EyeMovementDesensitizationandReprocessing,Obsessive-Compulsive
Disorder
1. Background for OCD, including exposure/response prevention (ERP).
However,oneofthemostcriticallimitationsofERPisthat
Inthediagnosticandstatisticalmanualof mentaldis- almost half of the patients do not respond to these treat-
orders(DSM-5),thefifthedition,obsessive-compulsivedis- ments,donotcompletetheirtreatment,orareresistantto
order (OCD), and similar related disorders are sorted in a it (4, 5). In otherwords,half of thepatientswithOCDshow
spectrum and classified as a separate subtype (1). In this signsof recoveryafterreceivingonecourseERP(6). Inde-
spectrum, OCD is the most problematic disorder, which tail, 75% to 80% of these patients report symptom reduc-
candisrupttheinterpersonal,occupational,andpersonal tion, and only 40% to 52% are cured (7-9). Besides, almost
life of the patientsimposingsubstantialeconomicandso- 25% of thepatientsfullycompletethetreatment(10).
cial costsontheindividualandsociety(2). Given the above problems, the question that arises is
The behavioral approach to OCD emphasizes on com- howtohelpOCDpatientsinwhomERPhasnothadasig-
pulsive behaviors that persist through negative reinforce- nificant effect, even in combination with medication (11).
ment (3). This theory recommends behavioral therapies Althougheyemovementdesensitizationandreprocessing
Copyright© 2020,Author(s).Thisisanopen-accessarticledistributedunderthetermsoftheCreativeCommonsAttribution-NonCommercial4.0InternationalLicense
(http://creativecommons.org/licenses/by-nc/4.0/)whichpermitscopyandredistributethematerialjustinnoncommercialusages,providedtheoriginalworkisproperly
cited.
SarichlooMEetal.
(EMDR) has already been supported empirically for the ever, regarding the application of this method in treating
treatmentof post-traumaticstressdisorder(PTSD),itsim- OCD,littleresearchisavailablesupportingitsimpact.
pact as an alternative treatment on OCD has also been ex- AlthoughtheuseofEMDRforOCDtreatmentwaspre-
aminedinrecentstudies. Several uncontrolled case stud- dicted by Shapiro and Forrest (24), few studies have used
iesandtworandomizedcontrolledtrialshavereportedthe this method combined with other interventions that are
successof usingEMDRtoreduceOCDsymptoms(11-14). effective in treating OCD (14). EMDR has also been shown
Preliminary studies have suggested that EMDR can be toinhibitserotoninreuptake(27);hence,thismethodcan
anappropriatealternativetreatmentforERPinOCD(15).To be useful in the treatment of obsessions. Considering
havedesirableprogressinthetreatmentofOCD,in-vivode- the specifications of OCD, the development of the EMDR
sensitization (exposure), and work on OCD-related events method and its combination with standard therapies to
usingEMDRtherapyshouldbeconsidered. Becauseof fo- help these patients are the main objectives of this study.
cusing on practical exercises in standard treatment, pa- Concerningafewstudiesonthistopic,theresultsofsmall
tientslearntoleavecompulsivebehaviorsandresistdoing case series cannot be generalized due to the lack of rig-
obsessivebehaviorsinreal-lifesituations. Withthehelpof orous design and susceptibility to biases. So far, only the
EMDRtherapy, they could better integrate the emotional experimental studies conducted by Nazari et al. (13) and
aspectsofproblemsandtransfertheiremotionallearning Marsden et al. (11) have empirically supported the use of
todailylifeandtolerateemotionaldistress. Therefore,the EMDRin the OCD treatment. However, in none of these
combination of EMDR with OCD standard treatment has studies, the presence of stressful life events has not been
beenintroduced(15-17).Resultsofstudieshaveshownthat considered in OCD patients under treatment. Further-
the combination of both methods can reduce OCD symp- more,intheaforementionedstudies,EMDRwasnotused
tomsinthelongterm.ComparedtoERPalone,thecombi- incombinationwithERP.
nationofEMDRandERPreducesthedropoutrateandcre-
ates higher motivation in patients (15). Like many psychi- 2. Objectives
atric disorders, OCD is also affected by stressful life events
both at the beginning and during the disease. Studies Consideringallthementionedpoints,inthisrandom-
have shown preliminary evidence about the relationship ized controlled trial, we attempted to examine the effects
between stress and OCD (18). Stressful life events in gen- of a combined serial protocol of ERP plus EMDR and its
eral andtraumas,inparticular,haveacontributiontothe comparison with standard ERP therapy in patients with
development of OCD symptoms both in the non-clinical OCDwhohavehadstressfullifeexperiences.
andclinical population through the creation of intrusive
thoughts and potential obsessive impulses (19). Studies
haveshownthatOCD,likePTSD,canbeinitiatedafterfac- 3. Methods
ingatraumaticexperienceorstressfulevent(20),andthe 3.1. Design
risk of OCD development in people with PTSD is 10 times
morethanthosewithoutproblemsrelatedtotrauma(21). Thecurrentrandomizedcontrolledtrial(RCT)wascar-
Therefore,peoplewithtraumaticandstressfulexperiences ried out using the parallel method, and with a pre-test,
aremorelikelytobediagnosedwithOCD(22,23). post-test, and follow-up design among OCD patients re-
In addition, obsessions/checking and symme- ferred to the outpatient clinic of 22 Bahman Hospital in
try/ordering are specifically associated with traumatic Qazvin after a psychiatrist’s diagnosis between April 2018
life events. Based on the model of adaptive information toMay2019.Thisstudycomplieswiththeguidelinesofthe
processing (AIP) in EMDR therapy, psychiatric disorders HelsinkiDeclaration.
are often the result of unprocessed traumatic events
(24). Although the presentations of OCD are different 3.2. Sampling
from that of PTSD, but there are some similarities, like UsingCohen’stable,thesamplesizewascalculatedas
repeated intrusive images and thoughts recalling anxi- 50 (25 for each group). According to this table, if the ef-
ety and extreme avoidance. Many case studies have also fect size is 0.50 at a significance level of 0.05, selecting
shownqualitative/metaphorical relationships among the 25 samples for each group can achieve the test power of
contents of obsessive intrusions. Emerging studies and 0.96. Consideringthepotentialdropout,30patientswere
hypothesessuggestthatEMDRmaybeausefultreatment randomlyassignedtoeachgroupafterinformedconsent
optionforOCD(25).Sinceitsintroduction,EMDRhasbeen formswereobtainedfromthem,andaccordingtothein-
utilized successfully for the treatment of psychological clusion/exclusioncriteria.Intheend,26patientsintheERP
consequencesrelatedtomanytraumaticevents(26);how- plusEMDRgroupand19intheERPgroupcompletedtheir
2 IranJPsychiatryBehavSci.2020;14(3):e101535.
SarichlooMEetal.
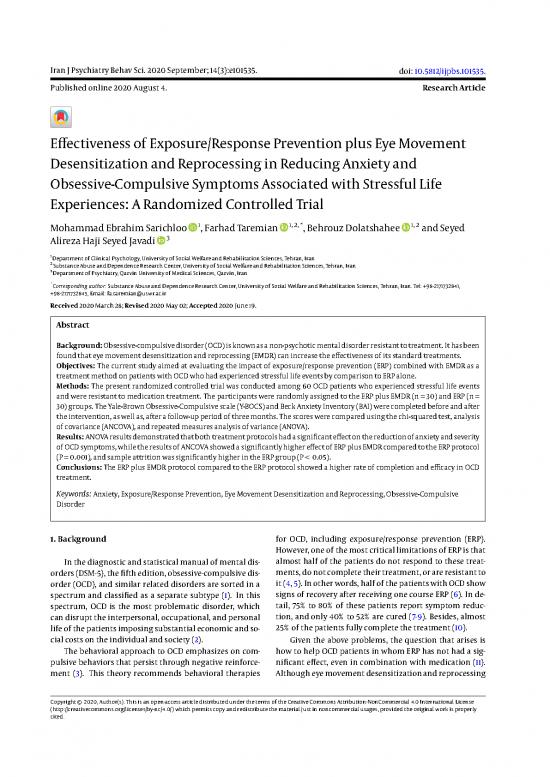
treatment. The flow diagram of participants in each ran- graphic characteristics, including education, marital sta-
domizedtrialstageispresentedinFigure1. tus, gender, age, job, the onset of the disorder, and history
The inclusion criteria were preliminary diagnosis of of obsessive-compulsivedisorderinthefamily.
OCD by structured clinical interview related to DSM-5
(SCID-5)(28),Y-BOCSscore≥ 16,having18-60yearsofage, 3.4.2. Structured Clinical Interview Related to DSM-5 (SCID-5-
having at least secondary education, lack of a comorbid CV)
disorder (any kind of psychological or medical disorder) TheSCID-5-CVscalefunctionsasacomprehensivestan-
noworinthepastexceptforsecondarydepression,having dardized tool to examine psychiatric disorders according
subclinical characteristics following OCD, not having sub- totheDSM-5definitionsandcriteriadevelopedforclinical
stance and alcohol abuse, not having attended any other investigation and research. Numerous studies in various
typesofpsychotherapiesoverthepastsixmonths,willing- countrieshaveconfirmedthereliabilityandvalidityofthe
ness to participate in the study (by completing a written instrument(28).
consentform),andhavingexperiencedaminimumofone
stressful life event (before the onset of OCD) according to 3.4.3. TraumaticExperienceChecklist(TEC)
thescoresofTraumaticExperiencesquestionnaire(TEC). This reliable and valid self-report instrument ad-
The exclusion criteria included having active suicidal dresses potentially traumatic events and can be used for
ideationandabsenceinmorethanonetreatmentsession. thepurposesofclinicalpracticeandresearch.Satisfactory
Based on these criteria, 60 samples were selected and as- indices belonging to the scale internal consistency and
signedtothetwogroupsofERPplusEMDR(n=30)andERP test-retest reliability confirmed the TEC reliability. Cron-
(n = 30) by the simple random sampling method. During bach’s alpha coefficients were 0.86 and 0.90 for the first
theinitialsessions,15samplesleftthestudyduetounwill- TECadministrationandtheTECretest,respectively(29).In
ingness to complete the treatment process (4 in the ERP astudyinIran,Cronbach’salphawascalculatedtobe0.62
plusEMDRgroupand11intheERPgroup).Theparticipants (30).
in both groups had a history of using the standard medi-
cationsforOCDtreatmentformorethansixmonthswith- 3.4.4. The Yale-BrownObsessive-CompulsiveScale(YBOCS)
out receiving adequate treatment response. At the time Goodmanetal.developedtheYBOCSasascalewith10
of the study, with the prescription of a psychiatrist, they itemsformeasuringOCDsymptoms.Itisscoredbetween0
werealsousingselectiveserotoninreuptakeinhibitors(SS- (nosymptom)and4(severesymptoms),withatotalscore
RIs). TheERPplusEMDRgroupreceived12sessionsofEMDR rangingbetween0and40.Itsinternalconsistencyis0.89
combinedwithERP,whiletheERPgroupreceivedonlyERP (11). In this study, we used the self-rated Y-BOCS designed
therapy;eachsessionlastedfor75-90minheldbyanexpe- byBaeretal.,whosecut-offscoreis≥ 16.Thisscaleiscom-
rienced cognitive-behavioral therapist (PhD candidate in monlyusedtodiagnosemoderatetoseveresymptomsof
ClinicalPsychology)with23years’ experienceinEMDRand OCD(31).Marsdenetal.(11)reportedaCronbach’salphaof
ERP(thefirstauthor).Therewasalsoonefollow-upsession 0.89fortheY-BOCS.IntheIranianversion,itsCronbach’sal-
threemonthsaftertheendoftreatment. phaisreportedtobe0.97(32).Inthisstudy,itwasobtained
Thecombinationofin-vivodesensitizationwithEMDR as0.76.
isdoneindifferentways.Thestandardmethodisusingthe
alternating technique (25). ERP and EMDR treatments are 3.4.5. The Beck Anxiety Inventory(BAI)
not combined in one session (15) and can be provided in Beck et al. (33) developed the BAI with 21 items. Each
alternatingsessions(17). itemreflectsoneofthecommonsymptomsofanxietyand
measuresitsseverityinthepastweek.Theitemsarescored
3.3. Ethical Considerations basedonaLikert-typescalebetween0and3,withthetotal
The current study was extracted from a PhD disser- score ranging between 0 and 63; scores between 0 and 21
tation on Clinical Psychology. The study was approved areindicativeof lowanxiety,between22and35areindica-
by the Ethics Committee of the University of Social Wel- tive of moderateanxiety, andequaltoandabove36repre-
fare and Rehabilitation Sciences (with the ethics code of senthighanxiety,whichrequiresfollowupandtreatment.
IR.USWR.REC.1396.301). TheBAIhashighinternalconsistency,andthecorrelation
betweenitsitemsfallswithintherangeof0.30-0.71(mean
3.4. Measures =0.60).ThePersianversionofBDIhashighinternalconsis-
3.4.1. DemographicCharacteristicsChecklist tency(α=0.92)andacceptablevalidityandreliability(34).
The checklist was developed by the researchers and Inthepresentstudy,aCronbach’salphacoefficientof0.89
used for the examination of the participants’ demo- wasobtainedforBAI.
IranJPsychiatryBehavSci.2020;14(3):e101535. 3
SarichlooMEetal.
Corresponding with 12 psychiatrists in the province (with
emphasis on the inclusion and exclusion criteria) for the
a
referral of patients with OCD ( N = 149 during 8 months).
76 identified from primary screening contacts
73 identified from waiting list
Screening and Exclusion:
1- U nwillingness to participate (n = 5)
Enrollment 2- N ot meeting inclusion or h aving exclusion
criteria (n = 11)
Eligible, consented
and randomized
(n = 60)
b c
Allocated ERP (n = 30) Allocated ERP plus EMDR (n = 30)
Allocation Continuation and completion of Continuation and completion of
treatment (n = 19) treatment (n = 26)
3- month follow-up (n = 19) 3- month follow-up (n = 26)
ollow-up
F
sis
Analyzed (n = 19) Analyzed (n = 26)
Imputed missing data = 0 Imputed mis sing data = 0
Analy
Figure1.CONSORTflowdiagram,obsessive-compulsivedisorder;A,exposure/responseprevention;BandC,eyemovementdesensitizationandreprocessing
3.5. Interventions lateral stimulation to elevate transition into a validated
3.5.1. EMDRwithERP positivecognition;(6)thisstepiscompletedwhenthepa-
tientcanbringthetargetmemoryandcognitionwithpos-
The EMDR is an eight-phase protocol: (1) Taking his- itive status to mind with no physical tension; (7) closing
toryandformulationofthecase;(2)preparationtoensure thesessionafterreductionof thepatient’stension; and8-
thattheclientshavethenecessaryresourcesforprocessing reassessment,whichisrepeatedatthestartofthenextses-
themanagementofdisturbinginformationtoachievean sion.
adaptivesolution;(3)addressingvisual,cognitive(desired
positive and negative cognition), sensory and emotional EMDRcanbeanappropriatechoiceforOCDtreatment.
elementsof recalls/thetargetmemoriesaredetected,and This study used the EMDR protocol proposed by Marr,
the level of disturbances and clients’ beliefs in cognition whichincludedtheprocessing of the current motivating
with positive status; (4) recalling the disturbing thought factors(obsessionsandcompulsionsofOCDconsideredas
ormemory(objective),andsimultaneously,performinga traumatic or current disturbing events), installing a pic-
set of eye movements(this procedure continues until the ture of the future (imagining successful actions in the fu-
subjective units of disturbance (SUD), and validity of cog- ture), and then processing disturbing events occurred in
nition(VOC)scalesscoresreachzero);(5)usingfurtherbi- thepast(17).
4 IranJPsychiatryBehavSci.2020;14(3):e101535.
no reviews yet
Please Login to review.